📌 MAROKO133 Update ai: Scientists build first breathing ‘lung-on-chip’ model using
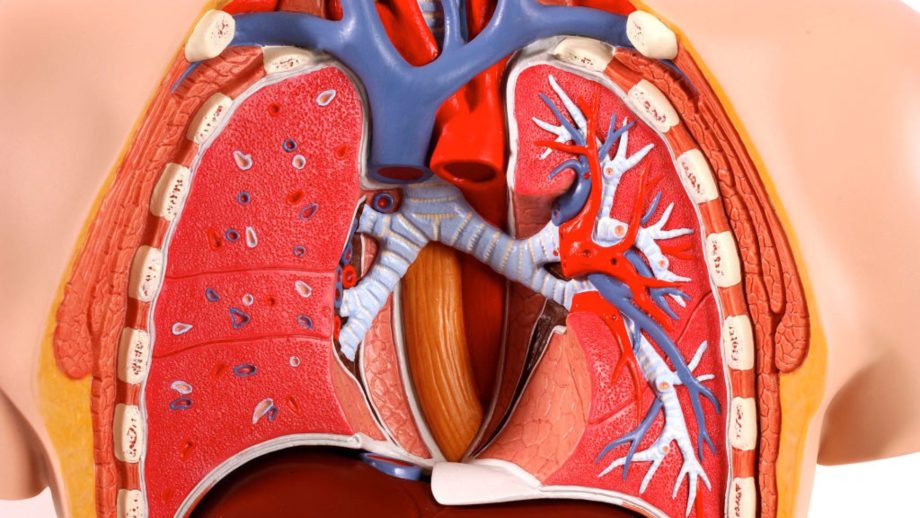
For the first time, a breathing lung model has been made using cells from only one person.
Announced on January 1, the development comes from researchers at the Francis Crick Institute in London and the Swiss company AlveoliX.
Notably, this “lung-on-chip” model will provide insights into Tuberculosis (TB) and perfect personalized medicine.
The chip acts like lung tissue. Because these chips can actually move like a breathing lung, researchers can use them to see how a specific person’s body fights TB, making it easier to find the right treatment for that individual.
“Given the increasing need for non-animal technologies, organ-on-chip approaches are becoming ever more important to recreate human systems, avoiding differences in lung anatomy, makeup of immune cells, and disease development between animals and humans,” said Max Gutierrez, Principal Group Leader of the Host-Pathogen Interactions in Tuberculosis Laboratory at the Crick and senior author.
Genetically identical cells
To better understand how the body fights respiratory diseases like flu and TB, scientists are developing “lung-on-chip” technology — miniature, plastic-housed units that replicate the air sacs (alveoli). This is where gas exchange occurs, and infections take hold.
Typically, these models were hampered by using a “mismatch” of cells from different sources, which failed to mirror a single person’s biology accurately.
By finally creating these chips using a single individual’s genetic profile, researchers can now precisely observe the unique battle between human cells and bacteria, something previously impossible.
This breakthrough uses induced pluripotent stem cells (iPSCs) to create a genetically identical miniature ecosystem.
“Composed of entirely genetically identical cells, the chips could be built from stem cells from people with particular genetic mutations. This would allow us to understand how infections like TB will impact an individual and test the effectiveness of treatments like antibiotics,” added Gutierrez.
To simulate life, the AlveoliX system uses rhythmic three-dimensional stretching. It pulls and pushes the tissue to mimic the expansion of a human breath.
This mechanical stress is vital. Without it, the cells don’t develop the tiny structures, known as microvilli, that are essential for lung function.
To simulate the infection, researchers populated the chip with donor-matched immune cells (macrophages) and introduced TB bacteria. This allowed them to witness the disease’s first moves within a single, consistent genetic environment.
TB disease replication
TB is a patient’s nightmare because of its stealth. It moves slowly. Months can pass between the first breath of bacteria and the first cough.
By adding the donor’s own immune cells (macrophages) to the chip, the team watched the war unfold in real time.
They witnessed “necrotic cores” — clusters of dead immune cells — forming five days before the entire lung barrier collapsed.
“TB is a slow-moving disease, with months between infection and the development of symptoms, so there’s an increasing need to understand what’s happening in the unseen early stages,” said Jakson Luk, Postdoctoral Fellow in the Host-Pathogen Interactions in Tuberculosis Laboratory and first author.
This technology offers a way out of the ethical and anatomical limitations of animal testing. Mice don’t breathe as humans do, and their immune systems don’t respond to TB the same way ours do.
While the current model focuses on TB, the team is already looking ahead. Flu, COVID-19, and even lung cancer could be the next targets for this tiny, breathing revolution.
The study was published in the journal Science Advances.
🔗 Sumber: interestingengineering.com
📌 MAROKO133 Update ai: Scientists Graft Human Ear Onto Foot Terbaru 2025
In a bizarre first, the South China Morning Post reports, doctors in China have surgically grafted a patient’s severed ear to her foot.
The patient, a woman identified by their surname Sun, suffered a horrific workplace accident involving heavy machinery which tore off a large part of her scalp and her ear with it, according to Qiu Shenqiang, deputy director of the microsurgery unit at Shandong Provincial Hospital in Jinan.
The damage to her scalp and vascular network was so severe that restoring the ear at the time was impossible, so the procedure was performed to save the patient’s aural orifice so it could be reattached to her head later.
The scalp, neck, and face had been torn and “split into multiple fragments, Qiu said, via SCMP, while the ear had been “completely severed along with the scalp.” The team tried to immediately repair it, but they came up against a grim medical reality: the skull needed more time — months, at least — to heal.
You can’t simply put a body part on ice for that long, so the surgical team opted for a radical approach: save the ear by attaching it to somewhere else on the body. Per SCMP, Qiu said they chose the foot because the arteries and veins there are compatible with those found in the ear. The foot’s skin and soft tissue are also similarly thin to the head’s.
The choice made sense in theory, but it was still a risk. Attaching a body part to a different site to preserve it, known as a heterotopic graft, is not uncommon during procedures like organ transplants. But doing this with an ear and foot had no precedent in medical history.
Nonetheless, Qiu’s team pulled it off. The initial grafting took ten hours, during which the surgeons meticulously connected the complex web of delicate veins.
But complications arose five days later, when the ear turned purplish black as its connecting veins struggled to send blood back to the heart, causing the blood to pool. Over the next five days, the team rescued the ear with manual bloodletting, a labor intensive process that required almost five hundred individual interventions.
Once the ear was stabilized, the team gradually restored the patient’s scalp. Five months on from the accident, the scalp and neck had healed enough, and the team returned the ear to its proper place.
The procedure was performed in October. The patient has now been discharged from the hospital, with her face and tissue function largely recovered, SCMP reported.
More medical news: People Jabbing Themselves With Black Market “GLP-3” Drugs
The post Scientists Graft Human Ear Onto Foot appeared first on Futurism.
🔗 Sumber: futurism.com
🤖 Catatan MAROKO133
Artikel ini adalah rangkuman otomatis dari beberapa sumber terpercaya. Kami pilih topik yang sedang tren agar kamu selalu update tanpa ketinggalan.
✅ Update berikutnya dalam 30 menit — tema random menanti!